Are GLP-1 medications the answer to perimenopause weight gain, or are we treating insulin resistance without addressing hormone shifts?

As a primary care and functional medicine physician with a specialty in perimenopause and menopause, I’ve watched the growing interest in GLP-1 medications for weight management during perimenopause with both excitement and caution. The hormonal shifts of perimenopause and into menopause can make weight gain feel inevitable, even with your best efforts at maintaining healthy habits.
Let me share how I approach these medications with my patients and how they might fit into your perimenopause journey.
Why GLP-1 Medications Are Suddenly So Popular
Semaglutide and Tirzepatide Explained
GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound)- the two most popular types- were originally developed for diabetes management. These injectable medications mimic incretin hormones, primarily glucagon-like peptide-1, which play a key role in regulating blood sugar, insulin secretion, appetite, fullness, and gastric emptying.
By improving insulin response after meals, reducing glucagon secretion, and slowing the rate at which food leaves the stomach, GLP-1 medications help to stabilize blood sugar levels and promote a prolonged sense of fullness. This often results in reduced caloric intake, decreased hunger and less blood sugar swings, thus leading to more effective weight loss.
In recent years, the remarkable effectiveness of these medications for significant weight loss has made brand names like Ozempic household words- and led to 13-17% of the U.S. population either being on or having tried these medications.
Clinical trials have shown participants losing 15-20% of their total body weight over a year—far more than what’s typically achieved with lifestyle modifications alone. For individuals with obesity or clear insulin resistance, this degree of weight reduction can meaningfully improve blood sugar control, blood pressure, inflammatory markers, and overall cardiometabolic risk.
Why Women in Their 40s Are Asking About Them
The menopause transition often brings stubborn weight gain- seemingly out of the blue-, particularly around the midsection. This isn’t always just about body size or appearance—it can also be about health.
Many midlife women find that despite maintaining their usual dietary choices/patterns, exercise levels, and physical activity, the scale keeps climbing. This frustrating shift has led many perimenopausal women to explore GLP-1 weight loss medications as a potential solution for hormonal weight gain.
So, the conversation becomes more nuanced in perimenopause. Many women in their 40s are not dealing with long-standing diabetes, but with shifting hormones, changing fat distribution, altered sleep, and emerging insulin resistance. This is where it becomes important to ask not just “Do GLP-1 medications work?” but “What problem are we actually trying to solve?”
Check out my Ultimate Guide to Perimenopause Symptoms guide here to learn more!
How GLP-1 Medications Work in the Body
Appetite Regulation and Satiety
GLP-1 medications work by mimicking the action of glucagon-like peptide-1, a hormone naturally released after eating. This effect helps reduce food cravings and increases feelings of fullness.
Many of my patients report that the constant thoughts about food (often referred to as “food noise”) simply quiet down. This makes maintaining a calorie deficit much more manageable during a stage of life when metabolism is changing (and often feels unmanageable).
Blood Sugar and Insulin Response
GLP-1 medications stimulate insulin release when blood glucose rises and suppress excess glucagon production. This helps stabilize post-meal blood sugar levels and reduces large glucose swings.
During perimenopause, fluctuating estrogen levels can worsen insulin resistance. As cells become less responsive to insulin, the body compensates by producing more of it. Elevated insulin promotes fat storage, particularly around the midsection.
By improving insulin dynamics, GLP-1’s help one of the underlying drivers of perimenopausal weight gain—not just the symptom of excess weight.
Slowed Gastric Emptying and Fullness Signals
GLP-1 medications also slow how quickly food leaves the stomach (gastric emptying). This prolongs feelings of fullness after meals and naturally reduces portion sizes.
For many women, this feels like relief from persistent hunger cues or cravings. However, this same mechanism contributes to common side effects of GLP-1 medications such as nausea, bloating, and constipation—especially when doses are increased. Careful titration and dietary adjustments are essential to tolerating these medications.
Why Weight Gain Feels Different in Perimenopause
Estrogen Fluctuations and Fat Distribution
As estrogen fluctuates and eventually declines, fat distribution shifts toward visceral storage—fat surrounding the abdominal organs. This change is not purely cosmetic.
Visceral fat is metabolically active. It increases inflammation, worsens insulin resistance, and raises long-term cardiovascular risk. The so-called “menopause belly” is a reflection of deeper metabolic shifts occurring beneath the surface that can be more damaging to health than it may appear.
Insulin Resistance in Midlife
Insulin resistance often accelerates during perimenopause. Cells become less responsive to insulin, leading to chronically elevated levels.
Higher insulin levels promote fat storage and make fat loss more difficult—even when caloric intake and exercise remain consistent. This explains why strategies that worked in a woman’s 30s may suddenly stop working in her 40s.
This is not a failure of discipline, though improved habits can make a difference. It is a change in physiology.
Sleep, Cortisol, and Metabolic Slowdown
Disrupted sleep is common in perimenopause, whether from night sweats, anxiety, or hormonal swings like estrogen dominance and declining progesterone. Poor sleep elevates cortisol, further impairing insulin sensitivity and promoting more abdominal fat.
The combined effect of estrogen shifts, sleep disruption, and elevated stress hormones creates a metabolic environment that feels resistant to effort. I often hear from women that they feel these changes are out of their control. Lack of sleep can also lead to increased cravings, particularly for low-density (processed or unhealthy carbs) or added sugar.
This is often the context in which women begin asking about GLP-1 medications.
When I Consider GLP-1 Medications for Women in Perimenopause
Clear Insulin Resistance or Rising A1c
When lab work shows rising blood sugar levels or evidence of insulin resistance, GLP-1 medications may offer benefits beyond weight management. Early intervention can help prevent progression to diabetes.
Many perimenopausal women show these metabolic changes years before receiving a diabetes diagnosis. GLP-1 therapy can be a helpful tool for improving metabolic health before more serious conditions develop. So, in certain cases, a GLP-1 medication can be an excellent fit to both help with weight loss and reduce cardiovascular and diabetes risk in the future.
Central Weight Gain Not Responding to Lifestyle Changes
When a patient has implemented consistent, evidence-based lifestyle changes—adequate protein intake, resistance training, blood sugar–supportive nutrition—and continues to gain visceral fat, GLP-1 therapy may be considered. But each woman must talk to their provider about the pros and cons, and make sure this is a good fit for them.
In this context, the goal is not cosmetic weight loss. It is metabolic risk reduction.
PCOS or Longstanding Metabolic Dysfunction
Women with polycystic ovary syndrome (PCOS) often struggle with insulin resistance throughout their lives. As they enter perimenopause, these metabolic challenges typically worsen and they often have a bigger struggle with perimenopause symptoms.
For these patients, GLP-1 medications can be particularly beneficial in managing the intensified metabolic shifts of perimenopause. The medications address the insulin resistance that has likely been a longstanding issue, and can help prevent further shifts into type II diabetes and/or heart disease.
When I Am Cautious About GLP-1 Use in Women Over 40
Low Muscle Mass or Inadequate Protein Intake
I’m cautious about prescribing GLP-1 agonists to women with already low muscle mass or poor protein intake. Rapid weight loss can accelerate muscle loss if not properly managed. This is one of the most common results I see when women start on GLP-1 agonists and don’t maintain or start an active strength training program and/or don’t focus on protein enough. For more info on starting a strength training program, check out this blog or this YouTube video:
Maintaining lean muscle mass becomes increasingly important after 40 for metabolic health, bone strength, and functional ability!
Bone Density Concerns
Women with pre-existing bone density concerns should be careful when considering taking a GLP-1 medication. Rapid weight loss and reduced nutrient intake can negatively impact bone health.
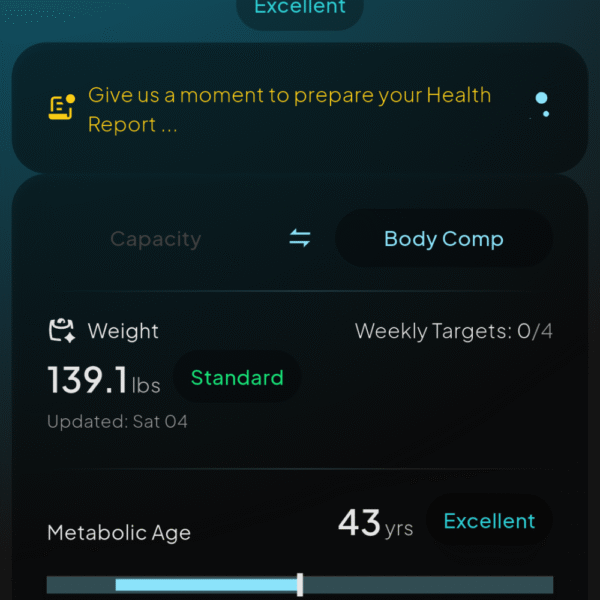
For these patients, I often recommend additional calcium and vitamin D supplementation, weight-bearing exercise 3-4 times per week for at least 30 minutes, and careful monitoring if we decide GLP-1s are appropriate. Protecting bone health is a critical aspect of the treatment plan, and it helps to have a way to measure muscle mass and bone health, like a BIA body composition device or a Hume Health Body Pod device that can assess bone health.
Learn more about the Body Pod in my Hume Health Body Pod Ultimate Review!
High Stress or Sleep Disruption
For women experiencing severe stress or significant sleep disruption, I often address these issues before considering weight loss medications. These factors can independently undermine metabolic health- meaning weight loss can be slower.
Improving sleep quality and managing stress are foundational to hormonal balance and weight management. Sometimes addressing these factors first leads to natural improvements in weight and metabolic health, even without the medication.
GLP-1 Medications and Muscle Loss in Midlife Women
Why Muscle Matters More After 40
Maintaining muscle mass becomes increasingly challenging—and increasingly important—after 40. Muscle tissue is metabolically active and supports insulin sensitivity. More muscle = a better metabolism and easier weight loss.
Loss of lean muscle mass contributes to the metabolic slowdown many women experience during perimenopause. Preserving muscle should be a priority in any weight management approach for women in this phase of life.
Protecting Lean Mass with Protein and Resistance Training
To counter potential muscle loss while using GLP-1 medications, I emphasize adequate protein intake and regular resistance/strength training. This combination helps preserve lean tissue during weight loss.
I typically recommend:
- Protein intake of at least 1.2-1.6g per kilogram of body weight daily (for pounds 0.55–0.75 grams per pound of body weight daily- for example, a 150-pound woman would aim for roughly 80–110 grams per day)
- Resistance training 2-3 times weekly
- Regular monitoring of body composition, not just scale weight- see above re: BIA and Hume Body Pod type testing
- Decreasing the dose of medication if muscle loss becomes concerning
Do GLP-1 Medications Fix Hormone Imbalance?
What GLP-1s Can and Cannot Fix
GLP-1 medications can improve metabolic health and reduce weight, but they don’t address the fundamental hormone changes of perimenopause. They’re not a replacement for hormone replacement therapy, if that is needed or appropriate for you.
For comprehensive symptom management, many women benefit from combining GLP-1 weight loss medications with menopausal hormone therapy. This approach addresses both metabolic changes and symptoms like hot flashes, vaginal dryness, and mood swings.
If hormone therapy is not right for you (and you must discuss this with your healthcare provider) a supplement blend like Happy Mammoth Hormone Harmony or FemGuard balance can help your menopause and perimenopause symptoms.

What Happens When You Stop GLP-1 Medications?
Risk of Weight Regain and Long-Term Strategy
Weight regain is common after discontinuing GLP-1 medications. Studies show that without a maintenance strategy, most people regain significant weight within a year of stopping. Studies show that after stopping GLP-1 medications, participants regain a significant portion of the weight they initially lost — in some trials, about two-thirds within a year.
A sustainable approach requires viewing these medications as tools within a broader lifestyle framework.
I work with patients to develop transition plans that may include:
- Slowly tapering the medication instead of stopping it suddenly
- Tightening up nutrition, protein intake, and strength training before coming off
- Discussing whether a lower “maintenance” dose makes sense for some women
- Addressing the hormone shifts and metabolic factors that were contributing in the first place
Rare Risks, Contraindications, and When GLP-1 Medications Are Not Appropriate
While GLP-1 medications are generally well-tolerated and highly effective for many patients, they are not appropriate for everyone.
Most side effects are gastrointestinal and dose-related — including nausea, constipation, bloating, reflux, or decreased appetite. These often improve with gradual dose titration.
However, there are also rare but important risks and contraindications to be aware of.
GLP-1 medications are not recommended for individuals with:
• A personal or family history of medullary thyroid carcinoma
• Multiple Endocrine Neoplasia syndrome type 2 (MEN2)
• A history of pancreatitis (in many cases)
• Severe gastroparesis or significant delayed gastric emptying
• Active gallbladder disease
There is also a small increased risk of gallstones, particularly with rapid weight loss. This is not unique to GLP-1 medications — rapid weight reduction from any cause can increase gallstone risk — but it is something to monitor.
In rare cases, pancreatitis has been reported. While large trials have not consistently shown a strong causal relationship, caution is still advised in patients with a prior history.
Because these medications significantly affect appetite and digestion, they must also be used carefully in women who are already under-eating, have a history of eating disorders, or are at risk for excessive muscle loss.
As with any medication, the decision to start a GLP-1 should be individualized.
These are prescription medications that require proper medical evaluation, lab monitoring, and follow-up. They should never be started without discussion with a licensed healthcare provider who understands both metabolic health and the unique physiology of perimenopause.
If you are considering a GLP-1 medication, talk with your provider about:
• Your metabolic markers
• Your muscle mass and bone health
• Your sleep and stress levels
• Your hormone status
• Your long-term strategy
A thoughtful, personalized plan is always safer — and more effective — than chasing trends.
Final Thoughts on GLP-1 in Perimenopause
GLP-1 medications represent a powerful tool for addressing the metabolic challenges many women face during perimenopause. When used appropriately, they can improve health markers and quality of life during this transitional phase.
However, they work best as part of a comprehensive approach that addresses the multiple factors affecting women’s health during this stage of life. The combination of appropriate medications, lifestyle modifications, and sometimes hormone therapy or herbal hormone support offers the most promising path for many women.
Every woman’s perimenopause experience is unique, requiring individualized care from a knowledgeable healthcare provider. If you’re considering GLP-1 medications, seek medical supervision from someone familiar with both these medications and women’s health.
With the right approach, this challenging phase of life can become an opportunity to establish health patterns that will serve you well into your postmenopausal years.
I recommend reading this next:
Perimenopause Symptoms: A Doctor’s Complete Guide to Relief

Dr. Shelley Meyer is a board-certified family physician and Institute of Functional Medicine-certified functional medicine physician, as well as a Registered Dietitian. She is passionate about helping women navigate the roller coaster of perimenopause and postmenopause. She has her own Functional Medicine Practice in Denver, Colorado.




Leave a Reply
You must be logged in to post a comment.